Understanding the Key Features of Intensive Outpatient Programs for Mental Health
Does a structured mental health treatment plan seem out of reach? This post explains what an IOP is, who it helps, and how it fits into a broader mental health treatment plan. It goes over key features of Intensive Outpatient Programs, targeted conditions treated, and what to expect during the program. Readers will understand the benefits of IOPs and learn how these programs address specific care needs reliably and efficiently.
Key Takeaways
- IOP integrates structured therapy with social work to support mental health
- Patients receive both personalized and group sessions with flexible scheduling
- Programs focus on building practical coping skills and managing behavioral challenges
- Treatment plans address substance abuse and provide clear guidance
- Family involvement enhances support and reinforces treatment outcomes
Understanding Intensive Outpatient Programs for Mental Health

This section defines intensive outpatient programs and explains their role in addressing disorders through varied treatment, including electroconvulsive therapy and managing suicidal ideation. It outlines how primary care and structured therapy work together to provide essential support for patients.
Defining Intensive Outpatient Programs and Their Purpose
Intensive outpatient programs offer structured mental health treatment through a coordinated approach that integrates therapy, social work, and support for what-we-treat issues, including substance abuse and coping difficulties. These programs provide a flexible, custom-designed framework that serves as a critical component of broader mental health recovery strategies.
Such programs focus on building practical coping skills and reinforcing daily functioning through regular therapy sessions and social work interventions. They emphasize tailored treatment plans that address both clinical symptoms and behavioral concerns, with specific attention to substance abuse challenges and life management strategies.
Key Features of Intensive Outpatient Programs

This section covers a structured treatment schedule with flexibility, advanced evaluation, and care levels that differ from other options. It details individual and group therapy, emphasizes skill development with coping techniques, and supports family education. Health insights include weight loss strategies, nurse practitioner input, and emergency department protocols to offer practical guidance.
Structured Treatment Schedule and Flexibility
The structured treatment schedule in intensive outpatient programs is designed to offer flexibility and meet specific patient needs, including those dealing with grief and emotional distress. The approach, which emphasizes setting clear goals, allows participants to maintain a consistent routine while balancing personal responsibilities, making it an attractive option in modern health care.
These outpatient programs provide an adaptable framework that supports various treatment objectives, ensuring that each individual’s goal is addressed with practical methods and real-world strategies. With a schedule that accommodates work and personal life, these settings empower participants to manage grief and other challenges efficiently, aligning treatment with overall health care priorities.
Level of Care Compared to Other Treatment Options
The content underscores that intensive outpatient programs provide a higher level of care compared to traditional treatment methods, integrating services such as nursing support and individualized medication management to prevent relapse. The approach can incorporate anger management strategies via in-person interactions and follow-up email communication to ensure continued progress.
These programs offer a unique blend of flexibility and structural support, which distinguishes them from more rigid inpatient care. The integration of nursing expertise, focused medication plans, proactive anger management, and routine email check-ins helps patients maintain stability and avoids potential relapse efficiently.
Integration of Individual and Group Therapy
The integration of individual and group therapy provides a balanced approach where personalized care meets collective support, addressing challenges related to the mind and overall mental health. This method supports suicide prevention and integrates insights from neurology and podcast discussions, offering an accessible resource for individuals covered by Medicaid and other services:
| Component | Detail |
|---|---|
| Individual Therapy | Focuses on personalized mental health care and direct support. |
| Group Therapy | Facilitates shared experiences and mutual understanding. |
| Integration | Combines one-on-one sessions with group dynamics to boost suicide prevention efforts. |
| Expert Insights | Utilizes neurology research and podcast advice for practical application. |
The combined therapy model delivers customized treatment plans while encouraging community involvement, resulting in efficient stress management techniques. Experts in behavioral health emphasize that this approach significantly benefits patients by addressing mental challenges through a cohesive care model that aligns with Medicaid protocols and innovative suicide prevention strategies.
Focus on Skill Development and Coping Mechanisms
The program’s emphasis on skill development provides participants with practical tools to support recovery, assist in managing alcohol-related challenges, and improve overall mood. Through strategies often aligned with employee assistance program protocols, professionals offer targeted support that complements structured therapy sessions.
By focusing on coping mechanisms, experts help individuals build resilience and maintain steady progress. The method incorporates guidelines from medicare and established practices from employee assistance programs to foster effective strategies that address mood fluctuations and recovery needs.
Support for Family Involvement and Education
The program fosters family involvement and education by actively incorporating clinician-led sessions that provide clear guidance on mental health treatment options, including strategies that account for health insurance details. This approach is designed to enable family members to support their loved ones effectively, benefiting not only patients but also first responder families who face unique challenges.
Family members are engaged through structured learning sessions that offer practical insights into mental health care, directly addressing common concerns and support strategies. The involvement of clinicians helps ensure accurate information is conveyed, enabling families to navigate treatment plans confidently, while also considering health insurance implications for comprehensive care.
Targeted Mental Health Conditions Treated in IOP

This section highlights targeted mental health conditions treated in IOP. It covers addressing anxiety disorders, managing depression effectively, supporting trauma recovery, treating substance use disorders, and specialized strategies for co-occurring challenges. The discussion provides practical insight into anger management, optimizing length of stay and behavioral outcomes at the clinic.
Addressing Anxiety Disorders
The program efficiently addresses anxiety disorders by integrating practical techniques with licensed physician oversight, ensuring that patients receive medical guidance tailored to their needs. The treatment combines conventional methods with supportive practices such as yoga to enhance relaxation and emotional balance.
The approach relies on comprehensive verification-of-benefits to ensure accurate coverage while offering additional support for conditions like schizophrenia and other related challenges:
| Aspect | Detail |
|---|---|
| Physician Support | Provides personalized medical guidance for anxiety and related conditions |
| Medical Oversight | Ensures treatment plans are tailored based on verification-of-benefits |
| Yoga Integration | Incorporates yoga sessions to help manage stress and promote health |
| Additional Services | Offers support for schizophrenia and other co-occurring disorders |
Managing Depression Effectively
The intensive outpatient program (iops) offers a structured environment where effective depression management techniques are combined with practical strategies to alleviate pain and prevent further injury; the program includes physical therapy elements and supportive counseling, ensuring that all participants, including those within the lgbtq community, receive targeted care and clear guidance on managing depression effectively:
| Aspect | Description |
|---|---|
| Depression Management | Structured therapy sessions and individualized support plans |
| Physical Therapy | Incorporation of exercises to reduce pain and improve recovery after injury |
| Inclusive Support | Specialized strategies for groups including lgbtq individuals |
The program emphasizes a proactive approach by integrating proven depression management practices with physical therapy to address pain and prevent additional injury; consistent application of these methods within iops paves the way for improved mental health outcomes and sustained overall recovery.
Supporting Recovery From Trauma
The program supports recovery from trauma by creating opportunities for patients to rebuild their lives through targeted mental health interventions, with a strong emphasis on building a supportive network. The treatment approach incorporates 988 hotline resources and specialized marketing techniques to promote awareness and timely assistance:
- Customized therapy sessions
- Access to network support
- Utilization of 988 services
- Engagement through targeted marketing
Experts in behavioral health integrate practical recommendations that include regular exercise routines and tailored PHP-based scheduling tools to track progress and refine treatment strategies. This combination of clinical expertise and actionable insights addresses patients’ pain points and aids in sustained recovery from trauma.
Treating Substance Use Disorders in IOP
The program employs a balanced approach to treating substance use disorders by integrating virtual care options, emergency interventions, and personalized medicine protocols. This integrated method supports patients facing challenges with addiction, ensures timely care, and offers adaptive treatment plans that prepare individuals for successful recovery:
| Component | Detail |
|---|---|
| Virtual Care | Accessible sessions that accommodate remote treatment needs |
| Emergency Interventions | Rapid response protocols during acute episodes |
| Personalized Medicine | Customized treatment plans to address unique recovery challenges |
The approach reflects clinical expertise, combining targeted therapies with support strategies for managing addiction and postpartum depression effectively. Patients benefit from a well-rounded treatment plan that emphasizes both structured therapy sessions and follow-up care to ensure lasting stability and improved mental health outcomes.
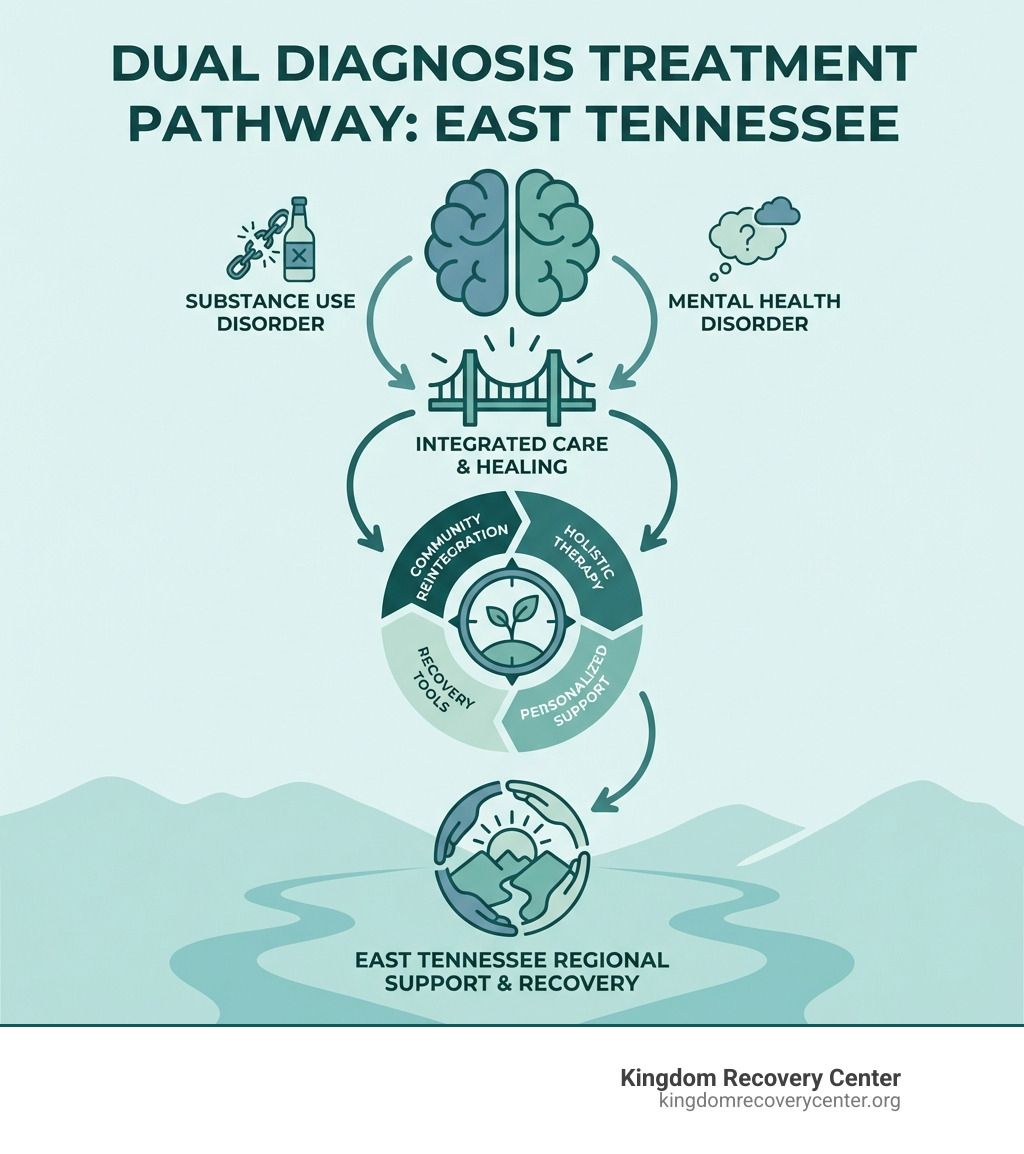
Specialized Strategies for Co-Occurring Disorders
Specialized strategies for co-occurring disorders in intensive outpatient programs blend behavior-focused treatments with vital support services, ensuring that individuals receive care that mirrors hospital and residential care approaches while emphasizing emotion regulation and stress management techniques. This method offers actionable insights to practitioners seeking effective ways to address mental and behavioral challenges, with a focus on achieving measurable outcomes and improved wellness:
| Component | Detail |
|---|---|
| Behavior Assessment | Evaluates patient responses to guide tailored interventions |
| Hospital Referral | Coordinates acute care when necessary |
| Residential Care Coordination | Integrates supportive transition options for higher care levels |
| Emotion Regulation | Offers techniques to manage emotional disturbances |
| Stress Management | Implements methods to reduce daily stress and improve coping skills |
The program emphasizes a structured approach that integrates proven behavior strategies with the supportive elements found in hospital and residential care, positioning emotion control and stress management as central goals. Such focused interventions provide a clear roadmap for patients and help sustain lasting improvements in overall mental health.
Benefits of Choosing an Intensive Outpatient Program

The program offers flexible scheduling for personalized treatment, ensuring continuous care benefits with a focus on effective management of health behavioral health challenges. It promotes strong social skills and encourages community engagement, much like a trusted medical center, to support recovery and ongoing well-being.
Flexible Scheduling for Personalized Treatment
The program offers flexible scheduling that allows each patient to create a personalized treatment plan, accommodating work responsibilities and life demands while providing dedicated therapy sessions. This customization enables individuals with varied gender identities to develop vital skill sets for managing stress and improving sleep quality, ensuring that treatment options such as tricare services are seamlessly integrated with regular patient care.
Flexible scheduling helps patients align therapeutic activities with their daily routines, facilitating consistent progress and addressing immediate issues as they arise. This approach supports the development of practical approaches to enhance skill and sleep improvement, providing balanced care in programs that consider diverse factors such as gender and tricare eligibility, which ultimately improves overall patient well-being.
Continuity of Care Benefits
Continuity of care in intensive outpatient programs provides a stable transition for patients who may have experienced inpatient treatment and now seek ongoing support for conditions such as bipolar disorder and other mental health diseases. This approach reduces the fear of treatment gaps by offering consistent access to vital information and services, ensuring that recovery is maintained through integrated therapy sessions and proactive follow-up.
Patients benefit from a seamless care plan that bridges the gap between acute management and long-term wellness, offering clear pathways for addressing mental health challenges. The structure of these programs allows individuals to build on their progress without the disruption often associated with switching from inpatient care to other treatment modalities, thus providing a secure framework for managing symptoms and reducing relapse risks.
Community and Peer Support in Recovery
Intensive outpatient programs in the united states often incorporate community and peer support to alleviate stress and advance education on mental health recovery. Health professionals emphasize that participation in art therapy sessions and peer-led groups significantly aids in building resilience and practical coping mechanisms:
- Collaborative workshops
- Peer mentoring opportunities
- Structured art therapy sessions
- Targeted community education events
These programs strengthen individual recovery through mutual support and expert guidance. By facilitating direct interaction among peers, participants gain actionable insights and practical strategies that help manage stress and maintain steady progress in their mental health journey.
What to Expect in an Intensive Outpatient Program

Patients in an IOP receive initial assessment and treatment planning, with defined duration and commitment levels. They experience smart recovery techniques and pharmacy consultations that boost motivation, along with approaches to measure progress and outcomes. Insurance and funding options are clarified to ensure practical treatment steps.
Initial Assessment and Treatment Planning
The initial assessment establishes a clear understanding of the patient’s current mental health status, using practical evaluation tools administered by experienced clinicians. This phase gathers essential information, such as symptoms, history, and goals, to shape a personalized treatment plan:
- Comprehensive symptom review
- Identification of treatment objectives
- Assessment of medical and behavioral history
The treatment planning process builds on the initial evaluation, setting measurable goals and scheduling therapy sessions tailored to individual needs. Experts ensure that each plan is designed to address specific challenges while accommodating personal circumstances, making the program accessible and effective for those requiring mental health services.
Typical Duration and Commitment Levels
Intensive outpatient programs for mental health typically run for several weeks to a few months, depending on the individual’s needs and progress, with a set schedule that accommodates regular therapy sessions and periodic evaluations:
| Aspect | Detail |
|---|---|
| Treatment Duration | Varies from 4 to 12 weeks based on structured therapy sessions |
| Commitment Levels | Requires participation several times a week along with regular assessments |
The program is structured to provide clear milestones and benchmarks for recovery, ensuring that every participant receives consistent support tailored to their daily responsibilities while achieving measurable progress in their mental health journey.
Therapeutic Techniques Used in IOP
Intensive outpatient programs utilize behavioral interventions and mindfulness exercises designed to promote practical recovery and symptom management. Clinicians employ structured therapeutic techniques that support personalized treatment plans, allowing patients to address their mental health concerns consistently and observe measurable progress over time.
In these settings, professionals combine cognitive methods with real-world strategies to address daily challenges and stress-related issues. Patients benefit from regular therapy sessions that focus on developing practical coping skills and fostering an environment that supports long-term mental well-being.
Measuring Progress and Outcomes in Treatment
Clinicians measure progress and outcomes in treatment by reviewing clinical assessments and patient feedback during regular sessions. A detailed tracking system outlines key indicators such as symptom reduction, functional improvement, and adherence to therapy protocols:
| Indicator | Description |
|---|---|
| Symptom Reduction | Measures improvement in clinical symptoms over time. |
| Functional Improvement | Assesses progress in daily functioning and routine management. |
| Therapy Adherence | Tracks consistency in attending therapy sessions and following treatment plans. |
Data derived from these measures support adjustments in treatment plans, ensuring that each patient receives targeted and effective care. This method provides clear insights into patient progress, empowering clinicians to address specific needs and improve mental health outcomes consistently.
Navigating Insurance and Funding Options for IOP
The program assists patients in understanding available insurance benefits and funding resources for mental health services. Experts help clarify policy details and guide patients in choosing coverage that aligns with their treatment needs, ensuring that cost is not a barrier to accessing intensive outpatient support.
Clinicians provide direct guidance on navigating insurance claims and exploring alternative funding strategies, such as grants and community programs. This approach empowers patients to secure the necessary financial support for their treatment journey and enhances their continuity of care.
Frequently Asked Questions About Intensive Outpatient Programs

This section answers key questions on how IOP differs from traditional outpatient care, identifies suitable candidates, explains cost factors, and explores the role of family support. It also covers possibilities for combining IOP with other therapies, offering practical insights for informed decisions about mental health treatment options.
How Does IOP Differ From Traditional Outpatient Treatment?
Intensive outpatient programs offer a more structured treatment schedule than traditional outpatient services, providing frequent therapy sessions and a focused approach to managing mental health challenges. This setup combines individual and group therapy sessions with continuous monitoring, resulting in a more dynamic and supportive treatment environment that addresses a range of symptoms effectively.
These programs differ by blending flexible scheduling with targeted interventions, which is particularly beneficial for individuals balancing work and personal responsibilities. The approach prioritizes hands-on, personalized care that actively tracks progress, making it an effective option for those seeking a comprehensive mental health treatment plan.
Who Is a Good Candidate for Intensive Outpatient Programs?
Individuals with manageable mental health symptoms who require structured support and flexibility in their treatment schedule are considered good candidates for these programs. This setting works well for patients who need targeted behavioral therapy without the more intensive demands of inpatient care.
Patients who balance professional and personal responsibilities often benefit from intensive outpatient programs, as these services provide consistent care and practical strategies for overcoming daily challenges. The model is particularly effective for those seeking comprehensive mental health support while maintaining their routine, ensuring that each step in recovery is well-guided and transparent.
What Are the Costs Involved With IOP?
The costs associated with intensive outpatient programs vary by provider and geographic location, with factors such as session frequency and therapy duration directly affecting overall pricing. Providers typically outline expenses during the initial assessment to ensure patients receive clear, upfront guidance.
Insurance coverage, sliding scale fees, and community programs may help reduce out-of-pocket expenditures for mental health services. A detailed breakdown of cost components is provided below for clarity and transparent comparison:
| Cost Component | Description |
|---|---|
| Session Fees | Charges per therapy session |
| Assessment Costs | Fees for initial evaluation and planning |
| Insurance Contributions | Portions covered by health insurance policies |
How Does Family Involvement Enhance IOP Success?
Family engagement enhances treatment outcomes by building a stable support network that reinforces therapeutic progress and encourages open communication. This involvement provides valuable insights for clinicians and offers patients reassurance through consistent participation from their loved ones.
Incorporating family members into the care process fosters a collaborative environment that supports accountability and promotes recovery goals:
- Active communication with mental health professionals
- Participation in educational sessions
- Shared understanding of treatment objectives
Can IOP Be Combined With Other Forms of Therapy?
Intensive outpatient programs can be effectively paired with other therapeutic methods to create a well-rounded mental health treatment plan. This integration allows providers to tailor interventions, ensuring that patient needs are met through a combination of structured sessions and additional support mechanisms.
Combining IOP with other treatments offers flexibility in care, enabling individuals to benefit from various approaches such as cognitive-behavioral therapy and mindfulness techniques. Such a combination enhances overall treatment outcomes by providing patients with multiple avenues to address their mental health concerns.
Conclusion
Key elements of intensive outpatient programs contribute substantially to mental health care by offering structured yet adaptable treatment environments. These settings integrate individual and group therapy to support both clinical symptoms and daily functioning. They also emphasize skill development, peer support, and family education to foster ongoing recovery. Overall, recognizing these features assists providers and patients in making informed decisions to manage mental health effectively.